What is Food is Medicine?
Food is Medicine is a holistic understanding of food as a living, relational pathway to healing and collective wellbeing, rooted in reciprocal relationships among land, water, people, ancestors, and spirit. When food is grown, gathered, prepared, and shared with reverence and cultural knowledge, it nourishes physical, mental, spiritual, and community health while sustaining balance and abundance for all beings.
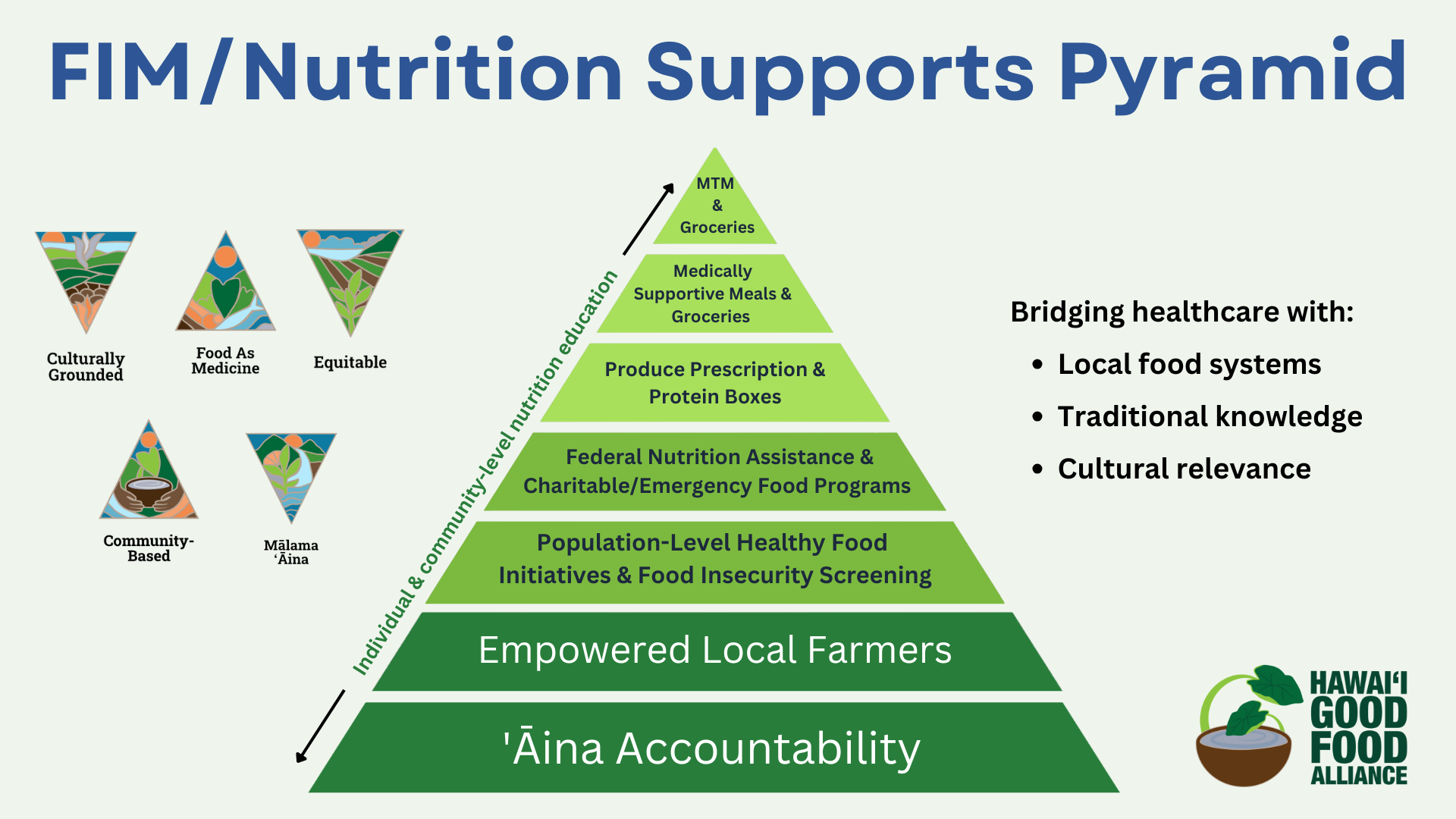
Our Approach in Hawai’i
Our approach to Food is Medicine is rooted in Hawaiʻi’s unique cultural values and local food landscape. In many indigenous cultures, including Native Hawaiian culture, the concept of “food is medicine” is a foundational truth – food is more than calories or nutrients; it is a direct connection to the ‘āina (land) and a source of spiritual and physical wellness. We embrace this perspective by ensuring that Hawaiʻi’s Food is Medicine initiatives honor local traditions, promote indigenous and local ingredients, and strengthen connections between people and their ʻāina. In Hawaiʻi, good food is understood as a cornerstone of health and well-being, and our programs reflect that understanding.
Beyond individual clinical care, we work on systems-level change to create a supportive environment for Food is Medicine. We often refer to this broader approach as “FIM+”, indicating an expansion of Food is Medicine to encompass food systems, culture, and policy. In alignment with HGFA’s guiding pillars, we ensure that:
Culturally relevant foods are included in all health interventions (honoring traditional diets and preferences). For example, produce boxes or meals provided through our programs feature local staples and culturally relevant foods whenever possible.
‘Āina Accountability: Local farmers and producers are integral partners in improving health outcomes. This means we prioritize sourcing from Hawaiʻi’s agricultural community, which not only supports farmers but also holds us accountable to the land – caring for the land that feeds us. Notably, Hawaiʻi’s recent Medicaid waiver explicitly encourages the inclusion of local growers, community gardens, and other community-based organizations in nutrition programs, helping strengthen Hawaiʻi’s food system through healthcare.
Sustainable Food Systems are built up through our work – we support local food procurement, infrastructure, and policies that make the healthy choice the easy choice. By investing in community food hubs, farmers markets, and local supply chains, Food is Medicine programs also bolster community food security and economic resilience.
Holistic, Community-Based Care is emphasized at every step. Our model integrates traditional knowledge, food sovereignty, and health equity principles. We recognize that healing is not just about individual patients, but about uplifting communities. Thus, we partner with community health centers, cultural practitioners, and social service organizations to address social determinants of health (like poverty and housing) alongside nutrition.
This comprehensive approach ensures that Hawaiʻi’s Food is Medicine efforts are grounded in local values while leveraging best practices from around the country. By uniting healthcare with local agriculture and community leadership, we strive to create a healthier, more food-secure Hawaiʻi for future generations. As HGFA’s Executive Director Kaiulani Odom has stated time and time again, connecting healthcare with our local food system – and fostering collaboration among doctors, community organizations, and farmers – is key to “building healthier communities rooted in ‘āina accountability”[21]. Our work embodies this philosophy in everything we do.
Why Food is Medicine?
Modern health challenges in Hawaiʻi and across the U.S. are closely linked to poor diet and food insecurity. Poor diet is now a leading cause of death nationally, contributing to high rates of chronic illness. Approximately one in seven U.S. households is food insecure, and fewer than 8% of Americans consume the recommended daily fruits and vegetables. As a result, diet-related conditions like hypertension, obesity, and diabetes have become widespread, driving up healthcare costs to an estimated $1.1 trillion per year in the U.S. Locally, thirty-two percent of Hawai‘i households (approximately 463,000 individuals) were food insecure in 2024–25.
Faced with these trends, healthcare innovators have turned to Food is Medicine (FIM) – a movement to integrate food and nutrition into healthcare in order to prevent, manage, and treat illness. FIM interventions connect patients with foods tailored to their medical needs through the healthcare system. In practice, this means health providers can “prescribe” healthy food just as they would a medication. Key Food is Medicine interventions include:
Produce & Protein Prescription Programs – Healthcare providers formally prescribe fresh fruits/vegetables and protein to patients, often delivered through vouchers or produce boxes, to encourage healthier diets as part of treatment.
Pantry Restocking/Healthy Meals - Healthcare providers formally prescribe groceries and pantry restocking to patients, also delivered through vouchers or produce boxes, to encourage healthier diets as part of treatment.
Medically Tailored Meals (MTMs) – Delivery of fully prepared meals designed by registered dietitians to meet the specific medical and nutritional needs of patients with serious health conditions (e.g. diabetes, heart disease). These meals are “tailored” to individual health needs and have been shown to improve disease management.
Nutrition Education & Counseling – Helping patients make informed food choices through nutrition classes, counseling sessions, and cooking education, so they have the knowledge and skills to support their health through diet and long-term behavior change.
Culturally Competent Care – Providing medical professionals with opportunities (classes, workshops, and community gatherings) to learn about place-based, Hawaiian and Pacific Islander food practices and nutrition, enhancing their ability to integrate food and health in a culturally grounded way.
Proven benefits
A growing body of research shows that Food is Medicine programs can significantly improve health outcomes and reduce healthcare costs.
For example, providing produce prescription benefits to food-insecure patients with diabetes is projected to prevent roughly 292,000 cardiovascular events and save $36.9 billion in healthcare expenses each year. Likewise, offering medically tailored meals to patients with diet-related illnesses could avert an estimated 2.6 million hospitalizations and save $23.7 billion annually in the U.S. These interventions not only address immediate food needs and clinical metrics, but also lead to fewer emergency visits and hospital stays by keeping patients healthier at home. In short, food is medicine because it leverages the power of nutrition to heal, ultimately improving quality of life and bending the healthcare cost curve.
According to recent research by Tufts University, the estimated net cost savings per patient participating in Medically Tailored Meal Treatment in Hawaii is $1,424 annually.